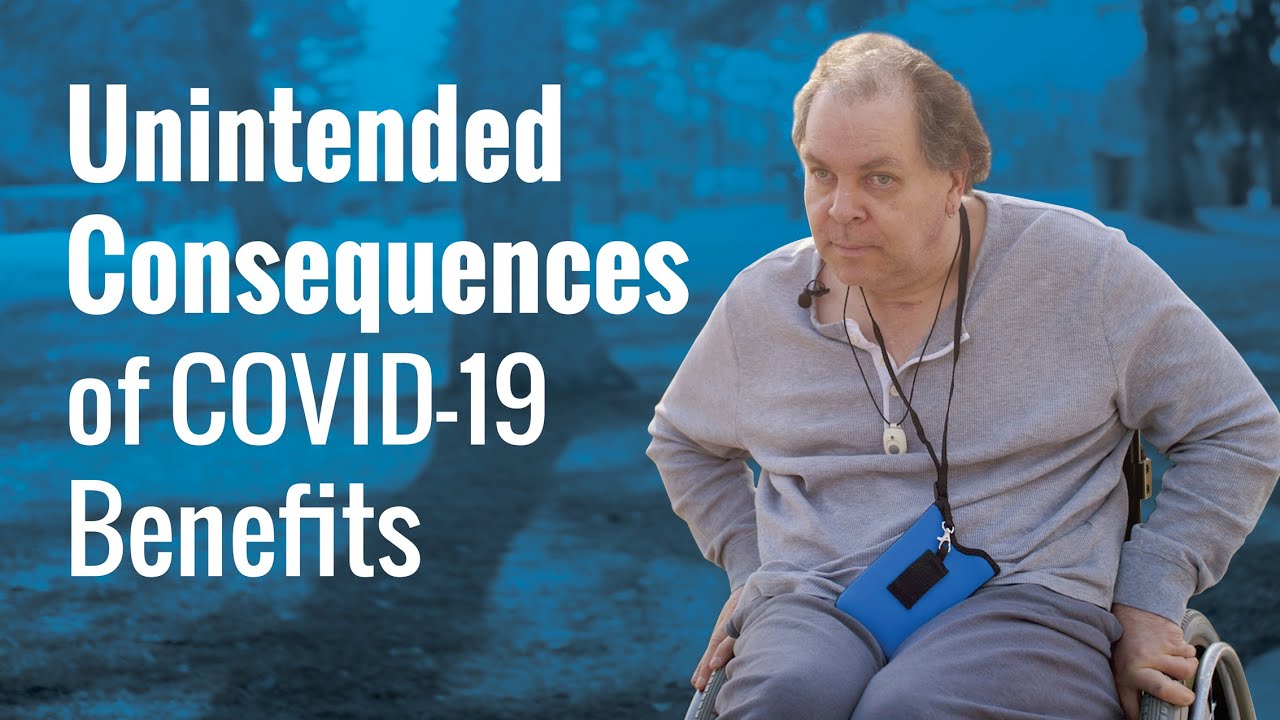
Growing up in Salt Lake City, Patrick Driscoll lived a normal life. His many aspirations included becoming a fireman, an archeologist, even a roller hockey player.
But at 19, like most others his age, Driscoll hadn’t yet figured out what exactly he wanted to do. He thought he had plenty of time to figure that out.
But on Sept.12, 1985, Driscoll’s life dramatically changed. He came down with a rare, infectious influenza that suddenly caused the epiglottis in his throat to swell up and block the airway to his brain.
His mother tried to give him the medication that his doctor had prescribed, but Driscoll was choking and couldn’t get it down.
Want to keep up with the 24/7 news cycle? Want to know the most important stories of the day for conservatives? Need news you can trust? Subscribe to The Daily Signal’s email newsletter. Learn more >>
“I thought I was just having a panic attack or just having a hard time breathing,” Driscoll recalls.
His mother tried to call his doctor, but he went into convulsions. When the ambulance arrived to take him to the hospital, paramedics had to perform triage to keep him alive.
When Discroll woke up, he was in an intensive care unit, unable to see or move.
“When I woke up in [the] ICU, I was totally blind,” Driscoll recalls. “I couldn’t see anything, just black.”
When he tried to pick up something to eat, he couldn’t get his hand to move at all.
Doctors eventually classified Driscoll as spastic quadriplegic with a vision impairment and a seizure disorder. His disability causes involuntary movements and affects all four limbs. Because he can’t see clearly enough to read, under Utah law he is legally blind.
Driscoll spent 19 days on a respirator in the ICU, seven months in rehab, and more than three years in nursing homes.
At the time, in the 1980s, nursing homes were the only facilities equipped to handle Driscoll’s level of disability. But he was only in his 20s, and nursing home life wasn’t for him. To find some sort of peace with his new reality, Driscoll decided he needed to live on his own.
To live independently in Salt Lake City, Driscoll depends on caregivers to show up to his home twice a day, in the morning between 7 and 7:30 and at night between 9 and 9:30. The caregivers help him with the most basic necessities—to get in and out of bed, shower, and prepare food.
“I actually wish they would’ve pulled the plug on me and let me die,” Driscoll, now 55, says of the challenge of relying on others for help. “I don’t like being dependent on people’s assistance to get up and do my [activities of daily living] or brush my teeth, wash my face, or shower. But in my case, I live alone and I need the help really bad.”
Driscoll was stricken with his condition after graduating high school.
Despite his disabilities, he began to attend the University of Utah in 1991, graduating 11 years later with a bachelor of arts degree in history in 2002. He got help from friends with papers, studied by listening to lectures and books on tape, and took his exams orally.
“It was hard. It really was,” he says in an interview at his home.
Every morning now, an aide puts on Driscoll’s headphones so he can take phone calls and listen to books and documentaries on tape. At night, an aide takes off his headphones and gets him into bed, where he remains until a caregiver shows up the next morning. Fingers crossed he can hold his bladder.
In addition to helping him meet these basic needs, Driscoll’s caregivers are supposed to administer his antiseizure medications every day at the same time.
But since COVID-19 hit, he says, many of his regular caregivers have been quitting or showing up late. Not because of the virus, but because of unemployment benefits in Utah during the pandemic that allow many workers to earn more from not working than from their usual wages.
Driscoll long has faced problems with the caregiving industry, where workers often are overworked and paid low wages. But ever since Congress allowed Americans to collect generous COVID-19 unemployment benefits instead of working, Driscoll says, the problems with his caregivers quitting or showing up late have gotten worse:
One of my caregivers said he was going to take the layoff and accept the money. Back then, they were getting $2,400 a month on top of what they were getting from this unemployment benefit as is. That’s a lot of money. I just don’t understand why they tried to kill businesses like they are doing with the extra money.
In response to the pandemic and government-forced business closures, Congress broadly expanded eligibility for unemployment benefits and loosened verification requirements. Lawmakers also added a $600-per-week federal bonus to regular unemployment benefits in Utah and other states.
With the extra $600 per week, University of Chicago economists estimated, 68% of unemployed workers received more in unemployment benefits than their usual wages.
“Normally, one cannot just claim they don’t want to work, as employers have to verify that a worker was actually laid off,” explains Rachel Grezler, a research fellow in economics, budget, and entitlements at The Heritage Foundation.
“However, under the Pandemic Unemployment Assistance program, which is open to self-employed individuals, gig workers, and others who don’t pay into the system, there are essentially no checks on eligibility,” Greszler said.
Jennifer Smith worked as Driscoll’s caregiver for more than four years through another company. They became friends and Smith now helps him with grocery shopping, food preparation, cleaning, prescription refills, and other needs that fall outside the scope of services provided by his official caregivers. Driscoll is able to pay her through a Medicaid program.
COVID-19 “has affected things a lot” for Driscoll, Smith says:
As far as his care, people don’t want to work. People don’t want to work because they make more money sitting at home. There was already a [certified nursing assistant] shortage, or even a caregiver shortage, going on before COVID happened. And now things are even harder for them to even staff people.
The Daily Signal and Independent Women’s Forum sought comment from Driscoll’s home care provider, Synergy HomeCare, about why his caregivers have been quitting or showing up late.
The company declined to comment.
Synergy HomeCare is a nonmedical home care agency operating throughout the U.S., serving roughly 25,000 clients, and employing about 20,000 people. All of its locations are independently owned and operated, and the one serving Driscoll is in Salt Lake City.
“I can’t speak for the office or what they’ve [got] going on behind the scenes. I just know it’s affecting my care when they don’t have staff to cover people, or when people call in sick or when they quit,” Driscoll says.
Smith says Driscoll is far from alone in what he’s experiencing.
“Patrick’s story is not one in a million,” she says. “There are a lot of people out there that are having problem[s] getting staffed, and they’re having problem[s] getting decent people who will listen.”
The Daily Signal and Independent Women’s Forum verified Driscoll’s account with two friends and two family members, all of whom receive his phone calls when his caregivers don’t show up on time.
“I get to know all my neighbors, just in case I need to get them to help me pick up something I dropped or I can’t find, or get me help if I have a seizure and end up on the floor,” Driscoll says.
One neighbor is an elderly man who, since COVID-19 hit, has regularly had to help Driscoll relieve himself after his caregivers show up hours late.
Over the past three months, “It’s almost turned into a weekly situation,” Driscoll says.
When somebody doesn’t show up, it affects his whole day and the next as well.
“Patrick limits how much he drinks, so that he can hold his bladder at night,” Smith says, adding:
And then during the next day, he won’t drink as much. And eventually it affects his health because he’s dehydrated. Patrick takes antiseizure medications and he’s on quite a high dose. And so seizure medicines should be taken at the same time every day. And that’s really difficult when people just show up whenever. He can have seizures, and he does have them when people don’t show up on time.
Over the past couple of weeks when his caregivers have been late, Driscoll says in the interview, “my little twitches, my spasms, are getting bad.”
“If I get my medicine for the next month or so on time, I shouldn’t have any problem,” he says. “But if it’s late a lot and with more time, it could cause me to have more adverse side effects. Have you ever seen somebody in a seizure?”
On March 12, Congress passed President Joe Biden’s COVID-19 relief plan, which continues the pandemic unemployment benefits but this time with a $300 weekly bonus on top of regular state unemployment benefits through September.
As of publication of this report, Patrick Driscoll’s caregivers from Synergy HomeCare were still showing up late, leaving him alone, unable to move from his bed.
>>> Independent Women’s Forum, which reported this story in partnership with The Daily Signal, works to develop and advance policy solutions that are targeted, fair, and improve Americans’ economic opportunities, freedom, and well-being. Learn more about Independent Women’s Forum here.